How Low-Dose Radiation Could Be The Trick For Treating COVID-19
Using low doses of radiation to treat the deadly inflammation of pneumonia, particularly viral pneumonia like that caused by COVID-19, was used during the first half of the 20th century with good results. And it may have a role in mitigating today’s pandemic.
Most discussions about the COVID-19 global pandemic, caused by the new coronavirus SARS-CoV-2, involve how to prevent spreading of the disease, as they should be.
The apparent 3% average case fatality rate of COVID-19 patients is quite large, although spotty testing makes it difficult to gauge. By comparison, seasonal flu generally kills far fewer than 1% of those infected. But it’s COVID-19’s contagiousness and increasing fatality rates with age that are so worrisome – increasing to 8% for patients aged 70 to 79 and 14.8% for those aged 80 and over.
Researchers are increasingly trying to develop methods to reduce these fatality rates. That means focusing on the 15 to 20% of people infected with COVID-19 who develop severe inflammatory effects that can lead to pneumonia, acute respiratory distress syndrome and death.
Using radiation may sound unusual, but it is currently being tested in clinical trials – using low doses of radiation to control lung inflammation. This method is being explored because severe COVID-19 cases causes cytokine release syndrome, also known as a cytokine storm.
Such a storm is a deadly uncontrolled systemic inflammatory response of the body’s immune system resulting from the release of great amounts of pro-inflammatory cytokines, which act as a major factor in producing acute respiratory distress syndrome, which is what kills.
It’s why we need ventilators and ICU beds so badly, and why this pandemic threatens to overwhelm our hospital systems.
Researchers are trying to target the pneumonia and stop or lessen the cytokine storm that leads to such high mortality rates. The problem is so acute that we seem willing to try anything to get a handle on this pandemic.
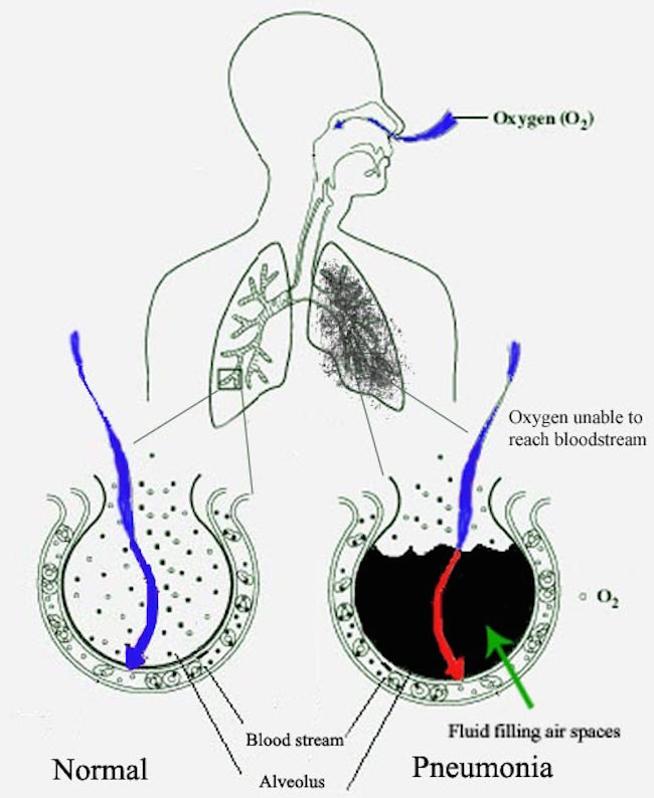
Pneumonia fills the lung’s alveoli with fluid, hindering oxygenation.
We were willing to try the anti-malaria drug, hydroxychloroquin, although it has not worked on COVID-19, has significant side-effects, and we don’t even know how it works on malaria. There are HIV protease inhibitors such as ritonavir and lopinavir, which have not yet shown much efficacy in early trials. Fortunately, Gilead’s remdesivir, an RNA dependent RNA polymerase inhibitor, has shown promise in human trials in shortening recovery times by a few days.
Other promising treatments involve taking blood plasma from recovered COVID-19 patients to collect antibodies to develop future treatments, track the virus or re-inject into sick patients.
But we also need to revisit past treatments that worked on pneumonia. Dr. E. J. Calabrese at the University of Massachusetts School of Public Health & Health Sciences and Dr. Gaurav Dhawan at the University of Massachusetts have discussed how X-ray therapy was used during the first half of the 20th century to successfully treat pneumonia.
In the first review, fifteen studies of about 700 cases of lobar and bronchopneumonia, sulfanilamide non-responsive, interstitial, and atypical pneumonia were effectively treated by low doses of X-rays.
Just this month, an additional article by them, along with other colleagues, covers the application to COVID-19 in greater detail. Studies from Germany also reviewed this method and its usefulness in addressing serious COVID-19 inflammation.
Oppenheimer first started to use X-ray treatments in 1943 for pneumonia patients, and Powell even earlier in 1939. Since then, low-dose radiation has been used for many medical applications, anything from cancer treatments to rheumatoid arthritis and other chronic autoimmune inflammatory diseases, that continue today.
It’s the anti-inflammatory effects of radiation, not its antiviral action, that could be invaluable to helping patients with COVID-19. And we are already completely set up for these radiation treatments at almost every hospital and cancer center – no new preparation, additional equipment, or training is needed.

Unfortunately, 70 years of irrational and unfounded fear of low doses of radiation, even those doses that occur naturally in the environment, have prevented testing of many of these treatments. Between the discovery of penicillin and the atomic bombs used in World War II, most interest in using radiation therapy for any disease other than cancer steadily waned.
Use of radiation therapy for non-neoplastic disease primarily continued in Germany, where it is still used for a wide variety of conditions.
Granted, radiation treatments that use very high doses, over 60Gy, carry some risks although those risks have been steadily declining with new approaches. Still, these risks are much less than the risks from the medical conditions they are treating.
But the doses that would be used to address the inflammation from COVID-19 will be much lower than those used for cancer treatments, only 0.1 to 1 Gy, and these doses carry little to no risk.
The gray, Gy, is a dose unit of ionizing radiation defined as the absorption of one joule of radiation energy per kilogram of matter.
There are researchers that do not see any value in this approach, but the field in general feels it deserves a closer look, and the medical community seems ready to test these treatments on humans with COVID-19.
Dr. Charles Kirby of the Department of Oncology at the University of Calgary and Dr. Marc Mackenzie of the Department of Oncology at the University of Alberta, review this approach recently in the Journal of Radiotherapy & Oncology.
Several medical institutions are set to start radiation therapies for COVID-19. Dr. James Welsh at Loyola University Medical Center, and former Chairman of the Board of the American College of Radiation Oncology and Editor-in-Chief of the Journal of Radiation Oncology, is moving to begin a national trial within the next few months on this treatment using low-dose radiation of 6 MV bremsstrahlung to the lungs.
Welsh notes there are several low dose radiation trials under consideration in the United States for people with COVID-19 pneumonia, and a similar number internationally.
The Clinicaltrials.gov website gives information on a trial already underway at Emory University and on an Italian clinical trial. A Spanish clinical trial has also just begun.
On March 20th, Dr. Jerry Cuttler, Emeritus from Atomic Energy of Canada Limited, wrote to the U.S. FDA and urged that a low-dose radiation trial be conducted at the Hines VA Medical Center in Chicago. His letter reached radiation oncologists in New York City, Moscow, New Delhi, Barcelona and Cape Town, South Africa. Radiation oncologists in Mexico and Argentina have also contacted him expressing interest.
Says Calabrese, “A possible mechanism by which low doses of radiation mitigates inflammation and facilitates healing is via the polarization of macrophages to an anti-inflammatory or M2 phenotype.”
The M1 type tends to overstimulate the immune system which can lead to a cytokine storm, while the M2 type tends to suppress the overreaction of the immune system.
 In addition, there are additional proposed mechanisms: inducing apoptosis, or directed purposeful cell death, in the most common white blood cells, radiosensitive neutrophils and activated immune cells, called T cells, and
In addition, there are additional proposed mechanisms: inducing apoptosis, or directed purposeful cell death, in the most common white blood cells, radiosensitive neutrophils and activated immune cells, called T cells, andinhibiting endothelial/leukocyte interactions resulting in reduced trafficking of infiltrating immune cells.
Past studies also show that low-dose radiation regulates lymphocyte counts, controls bacterial co-infections, and can modulate excessive inflammatory responses, exactly what is needed for COVID-19 patients.
The bottom line is that it’s all about our immune system. So a short primer might be warranted here. Our immune system defenses are of two types – innate and adaptive (or acquired). How the coronavirus affects these, and how radiation stimulates these, is key to this treatment. The M1/M2 changes are just part of it.
The major functions of the innate immune system include recruiting immune cells to sites of infection through the production of chemical factors, including cytokines, those specialized small regulatory proteins that are chemical mediators and signal the immune system to do specific things. When they get out of hand, bad things happen.
The adaptive immune system is activated through a process known as antigen presentation. T cells, both cytotoxic CD8 cells and CD4 cells, are part of the adaptive immune system. That is, they are target-specific and activated by antigen-presenting cells. Think of them as the “professionals” that get called in when there’s a big threat the local police can’t handle.
CD8 T cells directly kill malignant cells whereas CD4 T cells assist or hinder such killing. CD4 helper T cells generally work with CD cytotoxic T cells to eliminate things like cancers. CD4 regulatory T cells inhibit CD8 mediated cancer killing. If CD8 cells get out of control, then they can kill their own human so it’s essential that CD4 cells are there to stop that.
If radiation treatment helps balance this system and allows the inflammation to subside so that patients can continue to breathe for one or two weeks, then their adaptive immune system will have the opportunity to destroy all the infected cells.
There is another issue with coronaviruses in general – they are one of the few RNA viruses with a genomic proofreading mechanism which keeps the virus from accumulating mutations that could weaken it. It’s probably why common antivirals such as ribavirin, so effective against hepatitis C, have failed with this virus. These drugs weaken viruses by inducing mutations, but that won’t work for the coronavirus that proofreads its own RNA.
For more detailed information see Our Immune System and several of the links above. This is tricky stuff, but important if we want to understand this pandemic.
Dr. Mohan Doss, a Medical Physicist from Philadelphia, and Dr. Javad Mortazavi of Shiraz University of Medical Sciences, also looked at historic studies of low doses of radiation in the hopes of improving the immune response and reduce inflammation in COVID-19 patients (see Doss 2020 and Ghadimi-Moghadam et al., 2020).
These studies reported treating pneumonia patients by giving a very modest X-ray dose of about 0.3 Gy to the lungs. The average cure rate for all the studies was 83%. In one study by J. P. Rousseau et al., X-ray treatments of pneumonia patients dropped the fatality rate from 28% to 6%.

Most importantly for COVID-19, the radiation treatment was for viral pneumonia patients who had not responded to sulfonamides. COVID-19 causes viral pneumonia.
While antiviral drugs, anti-inflammatory drugs and statins are systemic drugs that affect the whole body, radiation treatments are able to specifically target the lungs where the inflammation occurs. None of the radiation doses used are at levels that cause significant health risks by themselves, and all are close to the range of Earth background radiation levels.
Separately, Mortazavi focused on low-level radiation treatments as a way to not mutate the virus into more drug-resistant forms.
This may strike you as counter-intuitive but, contrary to popular opinion and old wives’ tales, radiation is one of the weakest mutagens, and carcinogens, there is.
Low-dose radiation does not directly target the microbe, it targets the host’s immune reaction. Not so for biochemicals such as antivirals and antibiotics. These work directly against the offending microbes. If they clear each and every last virion, or infective particle, then they are successful.
But if they do not exterminate every last virion, there is a selective pressure that can cause them to evolve through mutations, strongly favoring survivors. It’s why we have so many drug-resistant infections.
In contrast to antiviral drugs, a dose of X-rays cannot exert a significant selective pressure on the SARS-CoV-2 virus and hence does not lead to resistance.
As we try lots of possible solutions to rein in the coronavirus SARS-CoV-2, we need to use every tool we have, and low-dose radiation therapy may be an important one. It would be unethical not to investigate this approach as thousands are still dying every day from this pandemic and a vaccine is a long ways off.